Traumatic Axonal Injury: Difference between revisions
(Created page with "== Traumatic Axonal Injury (TAI) Summary == === Definition and Mechanism === Traumatic axonal injury (TAI), previously known as diffuse axonal injury (DAI), occurs when shearing forces during acceleration or deceleration cause widespread microscopic axonal damage. This injury often results from rotational acceleration of the head, leading to shear, stretching, and compressive strains that deform brain tissue. TAI can occur without impact forces, although head impacts ty...") |
|||
| (One intermediate revision by the same user not shown) | |||
| Line 1: | Line 1: | ||
== Definition and Mechanism == | |||
Traumatic axonal injury (TAI), previously known as diffuse axonal injury (DAI), occurs when shearing forces during acceleration or deceleration cause widespread microscopic axonal damage. This injury often results from rotational acceleration of the head, leading to shear, stretching, and compressive strains that deform brain tissue. TAI can occur without impact forces, although head impacts typically exacerbate the injury. | Traumatic axonal injury (TAI), previously known as diffuse axonal injury (DAI), occurs when shearing forces during acceleration or deceleration cause widespread microscopic axonal damage. This injury often results from rotational acceleration of the head, leading to shear, stretching, and compressive strains that deform brain tissue. TAI can occur without impact forces, although head impacts typically exacerbate the injury. | ||
== Spectrum of TAI == | |||
TAI manifests in varying severities, from mild concussive syndromes to severe injuries associated with posttraumatic persistent vegetative states. The severity of TAI is graded based on macroscopic and microscopic lesions: | TAI manifests in varying severities, from mild concussive syndromes to severe injuries associated with posttraumatic persistent vegetative states. The severity of TAI is graded based on macroscopic and microscopic lesions: | ||
* '''Grade 1 TAI:''' Widespread axonal damage in the corpus callosum, cerebral white matter, [[brainstem]], and cerebellum. | * '''Grade 1 TAI:''' Widespread axonal damage in the corpus callosum, cerebral white matter, [[brainstem]], and cerebellum. | ||
| Line 10: | Line 8: | ||
* '''Grade 3 TAI:''' Includes Grade 2 findings plus small focal lesions in the rostral brainstem. | * '''Grade 3 TAI:''' Includes Grade 2 findings plus small focal lesions in the rostral brainstem. | ||
== Diagnosis and Imaging == | |||
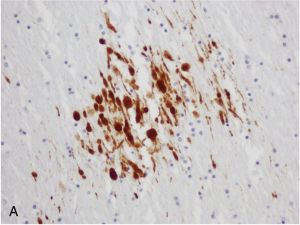
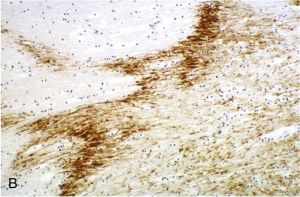
Neuroimaging techniques reveal the severity of TAI. Conventional imaging may not detect Grade 1 TAI, but Grades 2 and 3 may show visible hemorrhagic lesions in the corpus callosum and brainstem. Advanced techniques like immunocytochemical staining for amyloid precursor protein (APP) and neurofilament proteins help identify axonal damage more accurately. | Neuroimaging techniques reveal the severity of TAI. Conventional imaging may not detect Grade 1 TAI, but Grades 2 and 3 may show visible hemorrhagic lesions in the corpus callosum and brainstem. Advanced techniques like immunocytochemical staining for amyloid precursor protein (APP) and neurofilament proteins help identify axonal damage more accurately.<gallery widths="300" heights="300"> | ||
File:TAI-A.jpg|In traumatic axonal injury, amyloid precursor protein (APP)-immunopositive axonal injury shows a spectrum of axonal abnormalities, including axonal swellings, axonal retraction bulbs, and immunoreactive lengths (APP immunostain, corpus callosum; ×200). | |||
File:TAI-B.jpg|In vascular axonal injury, a zigzag pattern of amyloid precursor protein (APP)-immunopositive axonal injury occurs secondary to ischemia caused by internal herniation resulting from raised intracranial pressure (APP immunostain, corpus callosum; ×100). | |||
</gallery> | |||
== Pathophysiology == | |||
TAI involves the rapid accumulation of axoplasmic components and organelles at the injury site, leading to axonal swelling and eventual disconnection. This process results in axonal retraction bulbs and may lead to the formation of neuritic plaques. The mechanical loading of the brain, especially in midline structures like the corpus callosum and brainstem, is influenced by anatomical features like the falx cerebri and tentorium cerebelli. | TAI involves the rapid accumulation of axoplasmic components and organelles at the injury site, leading to axonal swelling and eventual disconnection. This process results in axonal retraction bulbs and may lead to the formation of neuritic plaques. The mechanical loading of the brain, especially in midline structures like the corpus callosum and brainstem, is influenced by anatomical features like the falx cerebri and tentorium cerebelli. | ||
== Clinical Implications and Interventions == | |||
TAI ranges from mild to severe, with varying recovery outcomes. Understanding the pathophysiological processes involved in TAI may offer insights into potential therapeutic interventions. Early identification and management of axonal damage could improve outcomes in TBI patients. | TAI ranges from mild to severe, with varying recovery outcomes. Understanding the pathophysiological processes involved in TAI may offer insights into potential therapeutic interventions. Early identification and management of axonal damage could improve outcomes in TBI patients. | ||
[[Category:Neurotrauma]] | |||
[[Category:Traumatic Brain Injury]] | |||
Latest revision as of 06:53, 20 July 2024
Definition and Mechanism
Traumatic axonal injury (TAI), previously known as diffuse axonal injury (DAI), occurs when shearing forces during acceleration or deceleration cause widespread microscopic axonal damage. This injury often results from rotational acceleration of the head, leading to shear, stretching, and compressive strains that deform brain tissue. TAI can occur without impact forces, although head impacts typically exacerbate the injury.
Spectrum of TAI
TAI manifests in varying severities, from mild concussive syndromes to severe injuries associated with posttraumatic persistent vegetative states. The severity of TAI is graded based on macroscopic and microscopic lesions:
- Grade 1 TAI: Widespread axonal damage in the corpus callosum, cerebral white matter, brainstem, and cerebellum.
- Grade 2 TAI: Includes Grade 1 findings plus focal abnormalities (usually small hemorrhages) in the corpus callosum.
- Grade 3 TAI: Includes Grade 2 findings plus small focal lesions in the rostral brainstem.
Diagnosis and Imaging
Neuroimaging techniques reveal the severity of TAI. Conventional imaging may not detect Grade 1 TAI, but Grades 2 and 3 may show visible hemorrhagic lesions in the corpus callosum and brainstem. Advanced techniques like immunocytochemical staining for amyloid precursor protein (APP) and neurofilament proteins help identify axonal damage more accurately.
-
In traumatic axonal injury, amyloid precursor protein (APP)-immunopositive axonal injury shows a spectrum of axonal abnormalities, including axonal swellings, axonal retraction bulbs, and immunoreactive lengths (APP immunostain, corpus callosum; ×200).
-
In vascular axonal injury, a zigzag pattern of amyloid precursor protein (APP)-immunopositive axonal injury occurs secondary to ischemia caused by internal herniation resulting from raised intracranial pressure (APP immunostain, corpus callosum; ×100).
Pathophysiology
TAI involves the rapid accumulation of axoplasmic components and organelles at the injury site, leading to axonal swelling and eventual disconnection. This process results in axonal retraction bulbs and may lead to the formation of neuritic plaques. The mechanical loading of the brain, especially in midline structures like the corpus callosum and brainstem, is influenced by anatomical features like the falx cerebri and tentorium cerebelli.
Clinical Implications and Interventions
TAI ranges from mild to severe, with varying recovery outcomes. Understanding the pathophysiological processes involved in TAI may offer insights into potential therapeutic interventions. Early identification and management of axonal damage could improve outcomes in TBI patients.