Traumatic Brain Injury Biomarkers: Difference between revisions
| (3 intermediate revisions by the same user not shown) | |||
| Line 12: | Line 12: | ||
== Protein Biomarkers == | == Protein Biomarkers == | ||
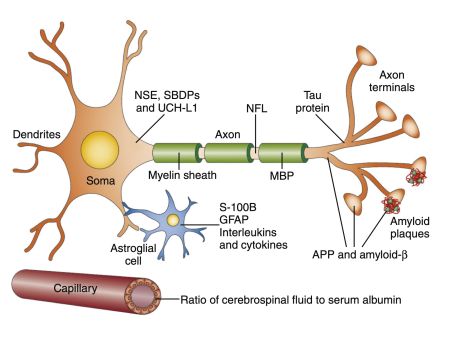
[[File:Screenshot 2024-07-20 at 9.01.41.jpg|thumb|452x452px|Markers of gray matter injury include neuron-specific enolase (NSE), αII-spectrin breakdown products (SBDPs), and ubiquitin C-terminal hydrolase-L1 (UCH-L1), all of which are proteins found in the neuronal cytoplasm. Markers of white matter injury may include glial fibrillary acidic protein (GFAP), S-100 calcium- binding protein B (S-100B), myelin basic protein (MBP), neurofilament polypeptides, and cleaved-tau protein. Overproduction of amyloid-β after trauma could result in formation of neurodegenerative pathology, while neuroinflammation may result in increased production of interleukins and cytokines. The integrity of the blood-brain barrier may be indicated by the ratio of cerebrospinal fluid to serum albumin. ''NFL,'' Neurofilament light polypeptide. (''From Zetterberg H, Smith DH, Blennow K. Biomarkers of mild traumatic brain injury'']] | |||
=== Neuronal Injury Markers === | === Neuronal Injury Markers === | ||
| Line 25: | Line 26: | ||
=== Neurodegeneration Markers === | === Neurodegeneration Markers === | ||
Tau proteins and amyloid-β peptides are linked to chronic traumatic encephalopathy and other neurodegenerative disorders following TBI. | Tau proteins and amyloid-β peptides are linked to chronic traumatic encephalopathy and other neurodegenerative disorders following TBI.<br clear="all"> | ||
== Dynamics of TBI Biomarkers == | == Dynamics of TBI Biomarkers == | ||
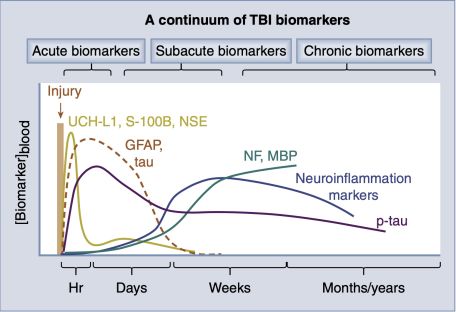
[[File:A continuum of TBI biomarkers.jpg|thumb|456x456px| '''Evidence-based time course of various key traumatic brain injury (TBI) biomarkers detected in blood following trauma.''' ''GFP,'' Glial fibrillary acidic protein; ''MBP,'' myelin basic protein; ''NF,'' neurofilament; ''NSE,'' neuron-specific enolase; ''p-tau,'' phosphorylated tau; ''S-100B,'' S-100 calcium-binding protein B; ''UCH-L1,'' ubiquitin C-terminal hydrolase-L1. (''Schematics modified from Wang KK, Yang Z, Zhu T, et al. An update on diagnostic and prognostic biomarkers for traumatic brain injury. Expert Rev Mol Diagn. 2018;18(2):165–180.'')]] | |||
=== Neuronal Injury Markers === | === Neuronal Injury Markers === | ||
| Line 46: | Line 46: | ||
'''Tau Proteins and Amyloid-β Peptides''': Tau proteins, especially their hyperphosphorylated forms, are associated with axonal damage and chronic traumatic encephalopathy. Elevated tau levels in CSF and serum after TBI correlate with injury severity, intracranial pressure, and poor outcomes. Amyloid-β peptides, resulting from the cleavage of amyloid precursor protein, accumulate following axonal damage. Although their role as acute markers is debated, they are implicated in long-term neurodegenerative processes post-TBI. | '''Tau Proteins and Amyloid-β Peptides''': Tau proteins, especially their hyperphosphorylated forms, are associated with axonal damage and chronic traumatic encephalopathy. Elevated tau levels in CSF and serum after TBI correlate with injury severity, intracranial pressure, and poor outcomes. Amyloid-β peptides, resulting from the cleavage of amyloid precursor protein, accumulate following axonal damage. Although their role as acute markers is debated, they are implicated in long-term neurodegenerative processes post-TBI. | ||
These biomarkers collectively offer a multifaceted view of the pathophysiological processes following TBI, enhancing diagnostic accuracy, prognostic assessments, and therapeutic monitoring. | These biomarkers collectively offer a multifaceted view of the pathophysiological processes following TBI, enhancing diagnostic accuracy, prognostic assessments, and therapeutic monitoring.<br clear="all"> | ||
== Clinical Applications and Future Directions == | == Clinical Applications and Future Directions == | ||
Latest revision as of 08:10, 20 July 2024
Importance
Biomarkers for TBI are crucial for improving diagnosis, prognosis, treatment, and monitoring of brain injuries, ranging from mild concussions to severe coma.
Clinical Validation
Biomarkers such as Ubiquitin C-terminal hydrolase-L1 (UCH-L1) and Glial Fibrillary Acidic Protein (GFAP) have shown promise in diagnosing TBI. The Banyan BTI test, which measures these biomarkers, received FDA clearance in 2018.
Pathophysiology
Biomarkers reflect the core pathophysiological elements of TBI, such as neuronal damage, white matter injury, neuroinflammation, and neurodegeneration.
Sampling Methods
Biomarkers can be measured in blood, cerebrospinal fluid (CSF), or saliva. Blood-based biomarkers are especially significant due to their ease of collection and potential for widespread clinical use.
Protein Biomarkers
Neuronal Injury Markers
- UCH-L1
- Neuron-Specific Enolase (NSE)
White Matter Injury Markers
- Glial Fibrillary Acidic Protein (GFAP)
- Myelin Basic Protein (MBP)
Neuroinflammation Markers
Inflammatory cytokines such as IL-1, IL-6, and TNF-α are assessed for their correlation with injury severity and neurological outcomes.
Neurodegeneration Markers
Tau proteins and amyloid-β peptides are linked to chronic traumatic encephalopathy and other neurodegenerative disorders following TBI.
Dynamics of TBI Biomarkers
Neuronal Injury Markers
Ubiquitin C-terminal hydrolase-L1 (UCH-L1): UCH-L1 is a neuronal injury marker detectable in both serum and cerebrospinal fluid (CSF) within one hour of traumatic brain injury (TBI). Increased levels of UCH-L1 correlate strongly with the severity of injury, the type and extent of lesions, and the necessity for neurosurgical intervention. High levels are also predictive of mortality within six weeks to three months post-injury. The ratio of GFAP to UCH-L1 is particularly indicative of diffuse axonal injury as opposed to focal hemorrhagic lesions.
Neuron-Specific Enolase (NSE): NSE is involved in glucose metabolism and is primarily found in neurons and neuroendocrine cells. Detectable in serum approximately six hours post-injury, NSE levels rise in response to severe TBI, correlating with poorer Glasgow Coma Scale scores upon hospital admission, higher mortality rates, and worse outcomes. However, NSE's sensitivity and predictive utility are less robust for mild TBI, and its levels can be significantly affected by hemolysis.
White Matter Injury Markers
Glial Fibrillary Acidic Protein (GFAP): GFAP is an intermediate filament protein found in astroglial cells, released following white matter injury. Elevated GFAP levels in both CSF and serum are associated with injury severity, high intracranial pressure, and poor functional outcomes. It is particularly useful in distinguishing between focal mass lesions and diffuse axonal injuries. The Banyan BTI test, which includes GFAP, provides diagnostic results within 4-6 hours post-injury.
Myelin Basic Protein (MBP): MBP is a component of the myelin sheath and is released into the extracellular matrix following white matter tract damage. Its levels in CSF and serum increase with the severity of TBI and are indicative of both axonal injury and blood-brain barrier disruption. However, MBP lacks specificity, as it can be elevated in chronic demyelinating conditions and normal aging.
Neuroinflammation Markers
Inflammatory Cytokines (IL-1, IL-6, TNF-α): Proinflammatory cytokines like IL-1, IL-6, and TNF-α are produced shortly after TBI, correlating with injury severity, intracranial pressure, and clinical outcomes. IL-6, in particular, has shown mixed results in predicting outcomes, sometimes correlating with both favorable and unfavorable results. The presence of these cytokines in the serum and CSF reflects the extent of the inflammatory response, although their specificity for brain injury is compromised by their elevation in other types of trauma and systemic inflammation.
Neurodegeneration Markers
Tau Proteins and Amyloid-β Peptides: Tau proteins, especially their hyperphosphorylated forms, are associated with axonal damage and chronic traumatic encephalopathy. Elevated tau levels in CSF and serum after TBI correlate with injury severity, intracranial pressure, and poor outcomes. Amyloid-β peptides, resulting from the cleavage of amyloid precursor protein, accumulate following axonal damage. Although their role as acute markers is debated, they are implicated in long-term neurodegenerative processes post-TBI.
These biomarkers collectively offer a multifaceted view of the pathophysiological processes following TBI, enhancing diagnostic accuracy, prognostic assessments, and therapeutic monitoring.
Clinical Applications and Future Directions
Diagnostic Panels
The combination of multiple biomarkers provides higher sensitivity and specificity for TBI diagnosis.
Proteomic Approaches
Advanced proteomic techniques allow for the simultaneous analysis of numerous biomarkers, aiding in the discovery of novel targets and improving the understanding of TBI pathophysiology.
Regulatory Milestones
The FDA approval of biomarker-based diagnostic tests marks a significant advancement in the clinical management of TBI, with more biomarkers expected to gain clearance in the near future.