Artery of Percheron: Difference between revisions
No edit summary |
No edit summary |
||
| (2 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
[[File:Artery of Percheron.png|thumb]] | {{NoteBox|info}} | ||
The '''artery of Percheron''' (AOP) is a rare anatomical variant (4-12% prevalence) of the posterior cerebral circulation, characterized by a solitary arterial trunk arising from one proximal [[Posterior Cerebral Artery|posterior cerebral artery]] (PCA) that supplies the bilateral paramedian thalami and often the rostral midbrain. In some cases, it also supplies the anterior thalamus. Infarction typically results from embolic occlusion, atherosclerosis, cardioembolism, or small vessel disease, leading to bilateral thalamic and mesencephalic infarcts. | =Key concepts= | ||
<ul> | |||
<li>Artery of Percheron is a rare variant in which a single artery arises from PCA to supply both thalami and the midbrain. Thrombosis can result in catastrophic bilateral stroke affecting consciousness and alertness </li> | |||
<li>Artery of Percheron is a variant in which a single artery arises from PCA to supply both thalami and the midbrain.</li> | |||
</ul> | |||
{{NoteBoxEnd}} | |||
[[File:Artery of Percheron.png|thumb]]The '''artery of Percheron''' (AOP) is a rare anatomical variant (4-12% prevalence) of the posterior cerebral circulation, characterized by a solitary arterial trunk arising from one proximal [[Posterior Cerebral Artery|posterior cerebral artery]] (PCA) that supplies the bilateral paramedian thalami and often the rostral midbrain. In some cases, it also supplies the anterior thalamus. Infarction typically results from embolic occlusion, atherosclerosis, cardioembolism, or small vessel disease, leading to bilateral thalamic and mesencephalic infarcts. | |||
== Clinical presentation == | == Clinical presentation == | ||
AOP infarction presents with a spectrum of symptoms due to involvement of thalamic and midbrain structures. Common features include altered mental status (drowsiness, agitation, obtundation, or coma), vertical gaze palsy, memory impairment (often with confabulation), and oculomotor disturbances. Additional signs may include hemiplegia, cerebellar ataxia, movement disorders (e.g., hemiballismus), and behavioral changes. Anterior thalamic involvement exacerbates memory deficits, while midbrain extension (mesencephalothalamic syndrome) adds cranial nerve palsies and motor issues. | AOP infarction presents with a spectrum of symptoms due to involvement of thalamic and midbrain structures. Common features include altered mental status (drowsiness, agitation, obtundation, or coma), vertical gaze palsy, memory impairment (often with confabulation), and oculomotor disturbances. Additional signs may include hemiplegia, cerebellar ataxia, movement disorders (e.g., hemiballismus), and behavioral changes. Anterior thalamic involvement exacerbates memory deficits, while midbrain extension (mesencephalothalamic syndrome) adds cranial nerve palsies and motor issues. | ||
Artery of Percheron occlusion ⇒ bilateral thalamic and mesencephalic infarctions | |||
== Diagnosis == | == Diagnosis == | ||
Latest revision as of 23:08, 27 July 2025
Key concepts
- Artery of Percheron is a rare variant in which a single artery arises from PCA to supply both thalami and the midbrain. Thrombosis can result in catastrophic bilateral stroke affecting consciousness and alertness
- Artery of Percheron is a variant in which a single artery arises from PCA to supply both thalami and the midbrain.
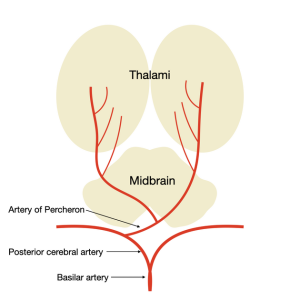
The artery of Percheron (AOP) is a rare anatomical variant (4-12% prevalence) of the posterior cerebral circulation, characterized by a solitary arterial trunk arising from one proximal posterior cerebral artery (PCA) that supplies the bilateral paramedian thalami and often the rostral midbrain. In some cases, it also supplies the anterior thalamus. Infarction typically results from embolic occlusion, atherosclerosis, cardioembolism, or small vessel disease, leading to bilateral thalamic and mesencephalic infarcts.
Clinical presentation
AOP infarction presents with a spectrum of symptoms due to involvement of thalamic and midbrain structures. Common features include altered mental status (drowsiness, agitation, obtundation, or coma), vertical gaze palsy, memory impairment (often with confabulation), and oculomotor disturbances. Additional signs may include hemiplegia, cerebellar ataxia, movement disorders (e.g., hemiballismus), and behavioral changes. Anterior thalamic involvement exacerbates memory deficits, while midbrain extension (mesencephalothalamic syndrome) adds cranial nerve palsies and motor issues. Artery of Percheron occlusion ⇒ bilateral thalamic and mesencephalic infarctions
Diagnosis
Imaging: MRI with DWI and FLAIR is diagnostic, revealing four patterns: (1) bilateral paramedian thalamic with midbrain (43%), (2) without midbrain (38%), (3) with anterior thalamus and midbrain (14%), (4) with anterior thalamus without midbrain (5%). Asymmetric involvement in 68%; "V" sign (hyperintensity along midbrain pial surface) in 67% of midbrain cases. CT shows hypoattenuation in affected areas. Synchronous infarcts possible in cerebellum, occipital lobe, or MCA territory. Histopathology/Angiography: Rarely needed; MRA/CTA may identify AOP variant or occlusion. DDx: Top-of-the-basilar syndrome, bilateral thalamic tumors/gliomas, deep cerebral venous thrombosis, encephalitis, or metabolic encephalopathy.
Treatment
Acute Management: Standard ischemic stroke protocol: IV thrombolysis (tPA) if within 4.5-hour window; endovascular thrombectomy for eligible large vessel occlusions. Supportive care including airway management for coma, blood pressure control, and antiplatelet therapy (aspirin/clopidogrel) for secondary prevention. Adjuvant: Statins for hyperlipidemia; anticoagulation if cardioembolic source (e.g., atrial fibrillation). Rehabilitation for motor/cognitive deficits. No routine neurosurgical intervention unless complications like hydrocephalus require shunting.
Prognosis and key points
Prognosis: Variable; mean age at presentation ~59 years (range 28-93). Complete recovery in ~26% (milder cases without midbrain/anterior involvement); persistent vigilance disorders, memory deficits, or motor issues in others. Memory often improves with time; mortality low but depends on infarct extent. Key Points: Prompt recognition critical for thrombolysis window. Preoperative imaging (MRA) useful in neurosurgical planning near thalamus/midbrain. Monitor for embolic sources; AOP variant increases risk of bilateral infarcts from single occlusion.