Dural arteriovenous fistula (DAVF): Difference between revisions
Jump to navigation
Jump to search
No edit summary |
|||
| (13 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
= Definition = | |||
* Acquired pathologic connections b/w dural art. and dural venous sinuses, meningeal veins, or cortical veins. | |||
= Epidemiology = | |||
* DAVFs account <10% of all [[Cerebral Vascular Malformations]]. | |||
* In US & Europe - majority involve the transverse sinus or sigmoid sinus | |||
** Japan - cavernous sinus MC | |||
= Etiology = | |||
* Idiopathic (MC), but have been assoc. w/ venous sinus thrombosis, meningitis, sinus infx, Qx, hypercoagulable states, trauma. | |||
== Pathogenesis == | |||
* venous sinus thrombosis → venous congestion & hypertension → upstream dilation of capillaries → arteriovenous shunting. | |||
* venous hypertension → ↓ perfusion → ↑ expression of vEGF → ↑ angiogenesis. | |||
= Pathology = | |||
* Lack a nidus on angiography. | |||
= DAVF Classification = | = DAVF Classification = | ||
The two most common classifications for dural AVFs are the Borden and the Cognard classification shown below: | * Several classification systems have been described to characterize DAVFs, with <span style="background-color:#fff2cc;">Borden and Cognard systems</span> being the most commonly utilized contemporary grading schemes. | ||
* <span style="background-color:#fff2cc;">Cortical venous drainage</span> is the defining angiographic feature that distinguishes benign (low-grade) from aggressive (high-grade) fistulas.</li> | |||
* Borden I, Cognard I, and Cognard IIa are considered low-grade, while all others are high-grade.</li> | |||
* The two most common classifications for dural AVFs are the Borden and the Cognard classification shown below: | |||
== Borden Classification == | == Borden Classification == | ||
[[File:Borden classification.jpg|thumb]] | |||
{| class="wikitable" | {| class="wikitable" | ||
!Type | !Type | ||
| Line 16: | Line 38: | ||
|III | |III | ||
|DAVF with direct retrograde flow from fistula into cortical veins, causing venous hypertension. | |DAVF with direct retrograde flow from fistula into cortical veins, causing venous hypertension. | ||
|} | |} <br clear="all"> | ||
{{NoteBox|info}}Borden classification has three types (Type I, II, and III), which can be remembered as "One, Two, Three". Each type's key feature can be remembered by the mnemonic: "Dura, Sinus, Brain" | |||
*<strong>Type I (Dura)</strong> - DAVF drains directly into dural venous sinus, with antegrade flow. It's a benign type, associated with lower risk. | |||
*<strong>Type II (Sinus)</strong> - DAVF drains into dural venous sinus, with reflux into the sinus. It's an intermediate type. | |||
*<strong>Type III (Brain)</strong> - DAVF drains retrogradely into cortical veins. It's a malignant type, associated with higher risk.{{NoteBoxEnd}} | |||
==Cognard Classification== | ==Cognard Classification== | ||
| Line 56: | Line 82: | ||
|Progressive myelopathy in 50% | |Progressive myelopathy in 50% | ||
|} | |} | ||
[[File:Cognard Classification.png|thumb| | [[File:Cognard Classification.png|thumb|600x600px|left]] | ||
<blockquote>Presence of cortical venous drainage is the most important determinant of rupture nsk from dural arteriovenous fistula. | <blockquote> | ||
The other factors listed have not been convincingly linked to risk of hemorrhage.</blockquote> | * Presence of cortical venous drainage is the most important determinant of rupture nsk from dural arteriovenous fistula. | ||
* The other factors listed have not been convincingly linked to risk of hemorrhage. | |||
* In the Cognard system, the <span style="background-color:#fff2cc;">pattern of venous drainage is the most critical factor</span>. | |||
*Lesions with retrograde flow in the cortical veins (IIb, IIa+b, III & IV) are considered <span style="background-color:#fff2cc;">high risk</span> for bleeding or intracranial hypertension. | |||
</blockquote><br clear="all"> | |||
{{NoteBox|info}}The Cognard Classification is more detailed, with five types (Type I, IIa, IIb, IIa+IIb, III, IV, and V). For Cognard, the mnemonic could be "Drain, Sinus, Brain, Both, Exhaust, Flow, Vein": | |||
* <strong>Type I (Drain)</strong> - DAVF drains into venous sinus with antegrade flow | |||
* <strong>Type IIa (Sinus)</strong> - DAVF drains into venous sinus with reflux | |||
* <strong>Type IIb (Brain)</strong> - DAVF drains into cortical vein | |||
* <strong>Type IIa+IIb (Both)</strong> - DAVF drains into sinus with reflux and cortical vein | |||
* <strong>Type III (Exhaust)</strong> - DAVF drains directly into cortical vein without venous ectasia | |||
* <strong>Type IV (Flow)</strong> - DAVF drains into cortical vein with venous ectasia | |||
* <strong>Type V (Vein)</strong> - DAVF drains into spinal perimedullary veins.{{NoteBoxEnd}} | |||
= Presentation = | = Presentation = | ||
<table> | <table class="wikitable" width="50%"> | ||
<tr> | <tr> | ||
<th>Sign/Symptom</th> | <th>Sign/Symptom</th> | ||
| Line 90: | Line 128: | ||
</table> | </table> | ||
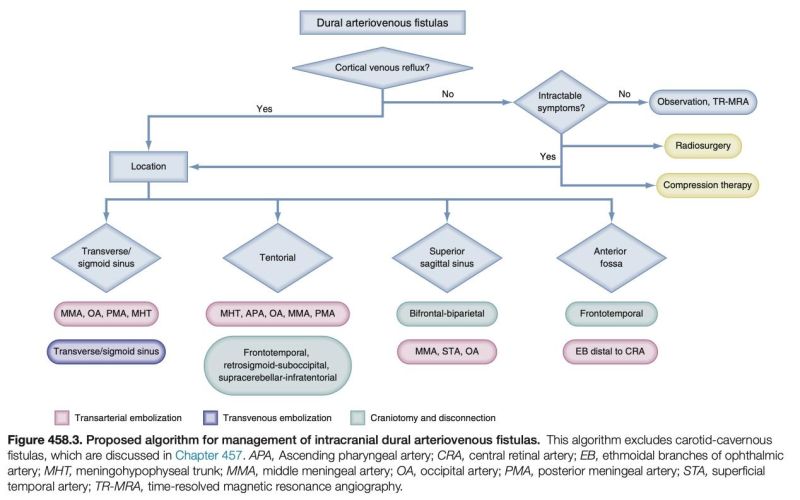
= Management of DAVF = | |||
[[File:Management of DAVF.jpg|center|frameless|800x800px]] | |||
[[Category:Vascular Pathology]] | [[Category:Vascular Pathology]] | ||
[[Category:Cerebral Vascular Malformations]] | |||
Latest revision as of 01:38, 3 March 2024
Definition
- Acquired pathologic connections b/w dural art. and dural venous sinuses, meningeal veins, or cortical veins.
Epidemiology
- DAVFs account <10% of all Cerebral Vascular Malformations.
- In US & Europe - majority involve the transverse sinus or sigmoid sinus
- Japan - cavernous sinus MC
Etiology
- Idiopathic (MC), but have been assoc. w/ venous sinus thrombosis, meningitis, sinus infx, Qx, hypercoagulable states, trauma.
Pathogenesis
- venous sinus thrombosis → venous congestion & hypertension → upstream dilation of capillaries → arteriovenous shunting.
- venous hypertension → ↓ perfusion → ↑ expression of vEGF → ↑ angiogenesis.
Pathology
- Lack a nidus on angiography.
DAVF Classification
- Several classification systems have been described to characterize DAVFs, with Borden and Cognard systems being the most commonly utilized contemporary grading schemes.
- Cortical venous drainage is the defining angiographic feature that distinguishes benign (low-grade) from aggressive (high-grade) fistulas.
- Borden I, Cognard I, and Cognard IIa are considered low-grade, while all others are high-grade.
- The two most common classifications for dural AVFs are the Borden and the Cognard classification shown below:
Borden Classification
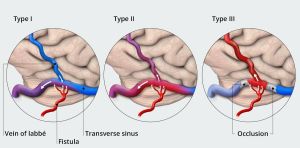
| Type | Features |
|---|---|
| I | DAVF drainage into a dural venous sinus or meningeal veins, with normal anterograde flow.
Usually clinically benign. |
| II | DAVF draining anterograde into dural venous sinus, but with retrograde flow into cortical veins. |
| III | DAVF with direct retrograde flow from fistula into cortical veins, causing venous hypertension. |
Borden classification has three types (Type I, II, and III), which can be remembered as "One, Two, Three". Each type's key feature can be remembered by the mnemonic: "Dura, Sinus, Brain"
- Type I (Dura) - DAVF drains directly into dural venous sinus, with antegrade flow. It's a benign type, associated with lower risk.
- Type II (Sinus) - DAVF drains into dural venous sinus, with reflux into the sinus. It's an intermediate type.
- Type III (Brain) - DAVF drains retrogradely into cortical veins. It's a malignant type, associated with higher risk.
Cognard Classification
| Venous drainage | Type | Features | Course |
|---|---|---|---|
| Sinus | I | Normal antegrade flow into a dural venous sinus | Benign course |
| IIa | Drainage into a sinus with retrograde flow within the sinus | Sinus reflux caused IC-HTN in 20% | |
| IIb | Drainage into a sinus with retrograde flow into cortical vein(s) | Reflux into veins induced hemorrhage in 10% | |
| IIa + b | Drainage into a sinus with retrograde flow within the sinus and cortical vein(s) | Aggressive in 66% with bleeding and/or IC-HTN | |
| Cortical veins | III | Direct drainage into a cortical vein without venous ectasia | Hemorrhage occurs in 40% |
| IV | Direct drainage into a cortical vein with venous ectasia | Hemorrhage occurs in 65% | |
| Spinal | V | Direct drainage into spinal perimedullary veins in addition to all of the above | Progressive myelopathy in 50% |
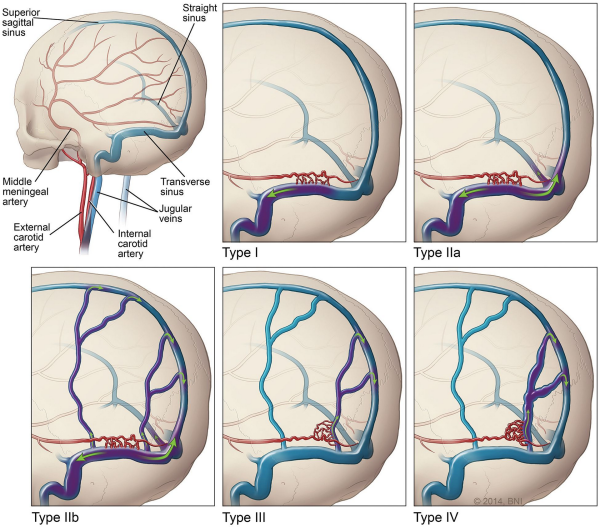
- Presence of cortical venous drainage is the most important determinant of rupture nsk from dural arteriovenous fistula.
- The other factors listed have not been convincingly linked to risk of hemorrhage.
- In the Cognard system, the pattern of venous drainage is the most critical factor.
- Lesions with retrograde flow in the cortical veins (IIb, IIa+b, III & IV) are considered high risk for bleeding or intracranial hypertension.
The Cognard Classification is more detailed, with five types (Type I, IIa, IIb, IIa+IIb, III, IV, and V). For Cognard, the mnemonic could be "Drain, Sinus, Brain, Both, Exhaust, Flow, Vein":
- Type I (Drain) - DAVF drains into venous sinus with antegrade flow
- Type IIa (Sinus) - DAVF drains into venous sinus with reflux
- Type IIb (Brain) - DAVF drains into cortical vein
- Type IIa+IIb (Both) - DAVF drains into sinus with reflux and cortical vein
- Type III (Exhaust) - DAVF drains directly into cortical vein without venous ectasia
- Type IV (Flow) - DAVF drains into cortical vein with venous ectasia
- Type V (Vein) - DAVF drains into spinal perimedullary veins.
Presentation
| Sign/Symptom | No. (%) |
|---|---|
| Pulsatile tinnitus | 25 (92%) |
| Occipital bruit | 24 (89%) |
| Headache | 11 (41%) |
| Visual impairment | 9 (33%) |
| Papilledema | 7 (26%) |
Management of DAVF