Dural arteriovenous fistula (DAVF): Difference between revisions
Jump to navigation
Jump to search
| Line 20: | Line 20: | ||
|III | |III | ||
|DAVF with direct retrograde flow from fistula into cortical veins, causing venous hypertension. | |DAVF with direct retrograde flow from fistula into cortical veins, causing venous hypertension. | ||
|} | |} <br clear="all"> | ||
<br clear="all"> | |||
{{NoteBox|info}}Borden classification has three types (Type I, II, and III), which can be remembered as "One, Two, Three". Each type's key feature can be remembered by the mnemonic: "Dura, Sinus, Brain" | {{NoteBox|info}}Borden classification has three types (Type I, II, and III), which can be remembered as "One, Two, Three". Each type's key feature can be remembered by the mnemonic: "Dura, Sinus, Brain" | ||
*<strong>Type I (Dura)</strong> - DAVF drains directly into dural venous sinus, with antegrade flow. It's a benign type, associated with lower risk. | *<strong>Type I (Dura)</strong> - DAVF drains directly into dural venous sinus, with antegrade flow. It's a benign type, associated with lower risk. | ||
Revision as of 23:47, 2 March 2024
DAVF Classification
- Several classification systems have been described to characterize DAVFs, with Borden and Cognard systems being the most commonly utilized contemporary grading schemes.
- Cortical venous drainage is the defining angiographic feature that distinguishes benign (low-grade) from aggressive (high-grade) fistulas.
- Borden I, Cognard I, and Cognard IIa are considered low-grade, while all others are high-grade.
- The two most common classifications for dural AVFs are the Borden and the Cognard classification shown below:
Borden Classification
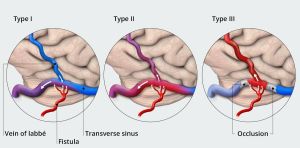
| Type | Features |
|---|---|
| I | DAVF drainage into a dural venous sinus or meningeal veins, with normal anterograde flow.
Usually clinically benign. |
| II | DAVF draining anterograde into dural venous sinus, but with retrograde flow into cortical veins. |
| III | DAVF with direct retrograde flow from fistula into cortical veins, causing venous hypertension. |
Borden classification has three types (Type I, II, and III), which can be remembered as "One, Two, Three". Each type's key feature can be remembered by the mnemonic: "Dura, Sinus, Brain"
- Type I (Dura) - DAVF drains directly into dural venous sinus, with antegrade flow. It's a benign type, associated with lower risk.
- Type II (Sinus) - DAVF drains into dural venous sinus, with reflux into the sinus. It's an intermediate type.
- Type III (Brain) - DAVF drains retrogradely into cortical veins. It's a malignant type, associated with higher risk.
Cognard Classification
| Venous drainage | Type | Features | Course |
|---|---|---|---|
| Sinus | I | Normal antegrade flow into a dural venous sinus | Benign course |
| IIa | Drainage into a sinus with retrograde flow within the sinus | Sinus reflux caused IC-HTN in 20% | |
| IIb | Drainage into a sinus with retrograde flow into cortical vein(s) | Reflux into veins induced hemorrhage in 10% | |
| IIa + b | Drainage into a sinus with retrograde flow within the sinus and cortical vein(s) | Aggressive in 66% with bleeding and/or IC-HTN | |
| Cortical veins | III | Direct drainage into a cortical vein without venous ectasia | Hemorrhage occurs in 40% |
| IV | Direct drainage into a cortical vein with venous ectasia | Hemorrhage occurs in 65% | |
| Spinal | V | Direct drainage into spinal perimedullary veins in addition to all of the above | Progressive myelopathy in 50% |
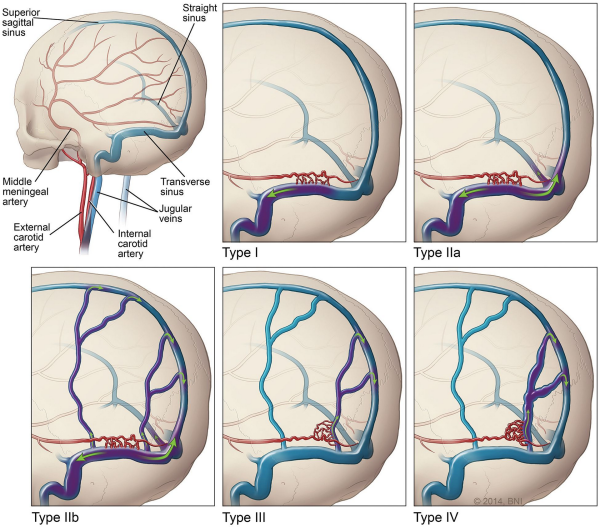
Presence of cortical venous drainage is the most important determinant of rupture nsk from dural arteriovenous fistula. The other factors listed have not been convincingly linked to risk of hemorrhage.
Presentation
| Sign/Symptom | No. (%) |
|---|---|
| Pulsatile tinnitus | 25 (92%) |
| Occipital bruit | 24 (89%) |
| Headache | 11 (41%) |
| Visual impairment | 9 (33%) |
| Papilledema | 7 (26%) |