Dural arteriovenous fistula (DAVF)
DAVF Classification
- Several classification systems have been described to characterize DAVFs, with Borden and Cognard systems being the most commonly utilized contemporary grading schemes.
- Cortical venous drainage is the defining angiographic feature that distinguishes benign (low-grade) from aggressive (high-grade) fistulas.
- Borden I, Cognard I, and Cognard IIa are considered low-grade, while all others are high-grade.
- The two most common classifications for dural AVFs are the Borden and the Cognard classification shown below:
Borden Classification
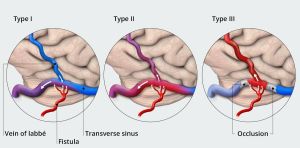
| Type | Features |
|---|---|
| I | DAVF drainage into a dural venous sinus or meningeal veins, with normal anterograde flow.
Usually clinically benign. |
| II | DAVF draining anterograde into dural venous sinus, but with retrograde flow into cortical veins. |
| III | DAVF with direct retrograde flow from fistula into cortical veins, causing venous hypertension. |
Borden classification has three types (Type I, II, and III), which can be remembered as "One, Two, Three". Each type's key feature can be remembered by the mnemonic: "Dura, Sinus, Brain"
- Type I (Dura) - DAVF drains directly into dural venous sinus, with antegrade flow. It's a benign type, associated with lower risk.
- Type II (Sinus) - DAVF drains into dural venous sinus, with reflux into the sinus. It's an intermediate type.
- Type III (Brain) - DAVF drains retrogradely into cortical veins. It's a malignant type, associated with higher risk.
Cognard Classification
| Venous drainage | Type | Features | Course |
|---|---|---|---|
| Sinus | I | Normal antegrade flow into a dural venous sinus | Benign course |
| IIa | Drainage into a sinus with retrograde flow within the sinus | Sinus reflux caused IC-HTN in 20% | |
| IIb | Drainage into a sinus with retrograde flow into cortical vein(s) | Reflux into veins induced hemorrhage in 10% | |
| IIa + b | Drainage into a sinus with retrograde flow within the sinus and cortical vein(s) | Aggressive in 66% with bleeding and/or IC-HTN | |
| Cortical veins | III | Direct drainage into a cortical vein without venous ectasia | Hemorrhage occurs in 40% |
| IV | Direct drainage into a cortical vein with venous ectasia | Hemorrhage occurs in 65% | |
| Spinal | V | Direct drainage into spinal perimedullary veins in addition to all of the above | Progressive myelopathy in 50% |
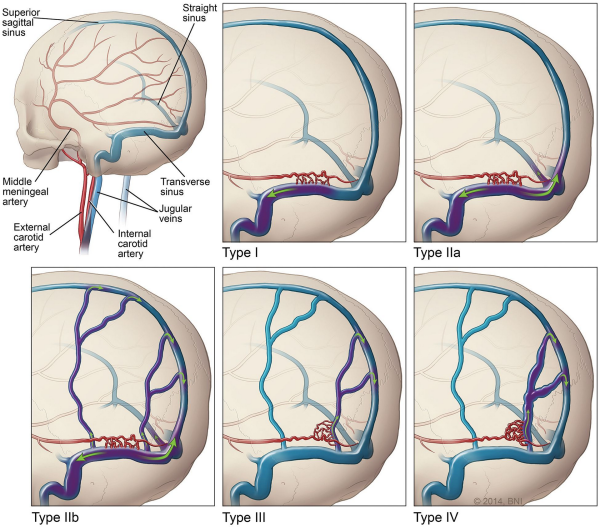
- Presence of cortical venous drainage is the most important determinant of rupture nsk from dural arteriovenous fistula.
- The other factors listed have not been convincingly linked to risk of hemorrhage.
- In the Cognard system, the pattern of venous drainage is the most critical factor.
- Lesions with retrograde flow in the cortical veins (IIb, IIa+b, III & IV) are considered high risk for bleeding or intracranial hypertension.
Presentation
| Sign/Symptom | No. (%) |
|---|---|
| Pulsatile tinnitus | 25 (92%) |
| Occipital bruit | 24 (89%) |
| Headache | 11 (41%) |
| Visual impairment | 9 (33%) |
| Papilledema | 7 (26%) |